Introduction
Trauma is one of the most important public health challenges worldwide. Following the advancement of science and technology and the industrialization of societies in the last century, trauma and its complications are now the most common causes of death and disability in people aged 1-44 (1,2).
Trauma is among the four leading causes of death in developing countries such as Iran and the second leading cause of death among young people (1,3). Iran has one of the highest mortality rates from road accidents. Every year, 27,000 deaths and approximately 240,000 injuries occur due to road accidents (4).
Trauma is a time-sensitive condition. Correct and effective management of trauma patients in pre-hospital and hospital settings helps reduce mortality and prevent complications (4). The main goals of managing trauma patients include quick assessment of critically ill patients, determining treatment priorities, and providing appropriate care services. Scoring systems are a tool used to achieve these goals. They are very useful tools for estimating patient outcomes such as mortality and trauma complications. The first scoring system for trauma patients was introduced approximately 60 years ago, but to date, many changes have been made (5).
There are two different types of trauma scoring systems. The first type is measured on the basis of the severity and anatomical location of the injuries. The Injury Severity Score is an anatomy-based score and was introduced in 1974 by Baker et al. (6). The second type of scoring system is based on the physiological response of the injured patient. One of the physiological scoring systems used to evaluate trauma patients is the revised trauma score (RTS). RTS was first designed and evaluated on the basis of a study with more than 2000 patients (7). The RTS consists of three physiological parameters: Glasgow coma scale (GCS), systolic blood pressure (SBP), and respiration rate (RR) (7,8).
In addition, two modified scoring systems, MGAP (mechanism of injury, GCS, age, and arterial pressure) and GAP (GCS, age, and arterial pressure) score, have been designed to predict survival in trauma subjects (3). GAP consists of Age, GCS, and SBP. The mechanism of injury is also included in the MGAP (9). Variables in GAP and MGAP are easily available at the time of admission. Regarding MGAP, there is a debate on how to score the mechanism of trauma. In this system, penetrating trauma is given a higher score, whereas penetrating trauma is not always more severe than blunt trauma (9,10). The scoring systems are effective not only in the appropriate triage of patients but also in predicting the severity of injury and mortality of patients (10-12).
The purpose of the present study was to evaluate and compare the diagnostic accuracy of RTS, GAP, and MGAP in predicting early in-hospital mortality of patients with multiple trauma referred to the emergency department (ED) in a regional trauma center in Rasht, Iran.
Materials and Methods
Study Setting and Design
This was a retrospective cross-sectional study that was conducted on patients with multiple trauma presenting to the ED of Poursina Hospital, Rasht, Iran, from March 2021 to December 2021. The study protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1400.519, date: 26.01.2022).
Participants
Adult multiple trauma patients with triage levels 1, 2, and 3 were eligible to participate in the study. The triage level was determined on the basis of the Emergency Severity Index (ESI) version 4 in the ED triage unit. ESI is a five-level ED triage modality that clinically classifies patients into five groups from 1 (most urgent) to 5 (least urgent) based on severity and resource requirements (1). Patients younger than 18 years who died before ED of, transferred from other medical centers, pregnant women, and those who had missing variables were excluded.
Data Gathering
Data were collected by reviewing patient case histories. The data included patient demographic characteristics (gender, age) and the mechanism of trauma at admission. The RTS, GAP, and MGAP scores were calculated according to the physiological variables (SBP, RR, and GCS) collected by the pre-hospital emergency system personnel.
Measurements
The RTS consists of three physiological parameters (GCS, SBP, RR). RTS=0.9368 GCS + 0.7326 SBP + 0.2908 RR. The total score is between 0 and 7.8408 (7). A lower RTS score indicates higher severity of the injury.
GAP consists of three parameters: physiological and age. The patient received 3 to 15 scores based on GCS score and three scores for age <60 years. They also received six scores for SBP >120 mmHg and four for SBP of 60-120 mmHg (13). The total score was between 3 and 24, with a lower score predicting a worse prognosis.
MGAP was calculated by adding the mechanism of trauma (blunt or penetrating) to the GAP score. The patient received 3 to 15 scores based on GCS score, five scores for ages 60 years, and four scores for blunt injury. They also received five scores for SBP >120 mmHg and three for SBP of 60-120 mmHg (9). Total scores ranged from 3 to 29, with higher scores being indicative of a better prognosis.
The primary outcome was early mortality. Early mortality was defined as patients who died due to multiple traumas within 24 h after admission to the hospital. The accuracy of the RTS, GAP, and MGAP scores with this outcome was investigated.
Statistical Analysis
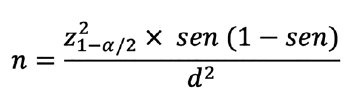
The minimum sample size was 245 subjects based on the results of a previous study (14) on the GAP score, assuming a sensitivity of 64%, a confidence level of 95%, and a type-2 error of 6%, according to the following formula: Sampling was performed using the consecutive sampling method.
Variables were analyzed using Statistical Package for the Social Sciences (IBM, Armonk, NY, version 21.0). Patient data were reported as frequency (%), mean±standard deviation (SD), or 95% confidence interval (CI). Fisher’s exact test, independent samples t-test, or Mann-Whitney U test were used to compare variables.
The area under the receiver operating characteristics curve (AUROC) was used to determine the discriminating power of the RTS, GAP, and MGAP to predict 1-day mortality. Sensitivity, specificity, positive and negative likelihood ratios, and positive and negative predictive values (PPV and NPV) were plotted for each score. P value <0.05 was considered significant.
Results
Two hundred and sixty-three multiple trauma patients were included. The mean (SD) age was 38.23 (15.75) years, and 82 (31.2%) patients were female. The 24-h mortality rate was 19 patients (7.2%). Motor vehicle accidents were the leading cause of injury (60.5%). Baseline characteristics are reported in Table 1.
The median (interquartile range) RTS, GAP, and MGAP scores were 7.1 (6.17-7.84), 21 (18-22), and 24 (22-27), respectively. The RTS, GAP, and MGAP scores were significantly higher in the survived patients than in the non-survived patients (p<0.001). The survived and non-survived patients had significant differences in age (p=0.004), SBP (p<0.001), heart rate (p=0.001), and GCS (p<0.001).
The AUROCs of RTS, GAP, and MGAP scores to predict 24-h mortality were 0.921 (95% CI: 0.882-0.951), 0.909 (95% CI: 0.867-0.941), and 0.898 (95% CI: 0.855-0.932), respectively (Figure 1). The optimal cut-off points for the RTS, GAP, and MGAP scores were ≤5.98, ≤18, and ≤21. The RTS, GAP, and MGAP scores were good predictors of 24-h mortality. RTS was similar to GAP (p=0.533) and MGAP (p=0.289) in predicting 24-h mortality. The NPVs of RTS, GAP, and MGAP for 24-h mortality were 99.0%, 99.0%, and 98.5%, respectively (Table 2).
Discussion
The primary goal of trauma patients is their survival. Therefore, identifying patients at risk of death is important. For this purpose, triage and scoring systems have been used to identify critically ill patients. These systems are effective not only in determining the prognosis of trauma but also in predicting the severity of the injury (6,14,15). The first scoring system for trauma patients was presented approximately 60 years ago, but there have been many changes in this field until today (5).
These scoring systems have limitations and benefits. A good scoring system should have fewer parameters, be easier to use, and be more accurate, especially in emergencies (15). In most multiple trauma patients, the severity of the injury and risk of death can be determined on the basis of physiological parameters in the scene (13). GAP was defined by Kondo et al. (13) in Japan. The GAP score is easy to use and calculate to determine trauma severity in the early stages (11). The MGAP score was developed by Sartorius et al. (16) as an improvement over the previous trauma scoring systems in France. Another scoring system is RTS, which has limited popularity due to the difficulty of calculation (13,16).
In addition, all scoring systems evaluated in this study (GAP, MGAP, and RTS) are heavily weighted on the GCS to compensate for significant head trauma without multisystem trauma or major physiologic changes. In this study, the predictive value of the three scoring systems in predicting early mortality within 24 h after admission was evaluated. The RTS, GAP, and MGAP scores were good predictors of 24-h mortality, and there was no significant difference between the three scores in predicting early mortality in multiple trauma patients.
In previous studies, a comparison of the scoring systems mentioned above has been made, but in most of them, one-month mortality or in-hospital mortality was considered. Similar to this study, Ahun et al. (11) compared RTS, GAP, and MGAP for short-term (24 hours) mortality prediction. They found that these scores were significantly associated with short-term mortality. AUROCs were 0.727 for RTS, 0.970 for MGAP, and 0.910 for GAP. The AUROC of MGAP to predict mortality was significantly higher than that of RTS, but there was no significant difference between MGAP and GAP (p=0.177). A multi-center study conducted in Kenya on 16,548 patients demonstrated statistically significantly higher performance of MGAP and GAP than RTS for in-hospital mortality (17).
Farzan et al. (6) reported that MGAP, GAP, and RTS accurately predicted one-month mortality in multiple trauma patients. RTS had slightly better AUROC than GAP and MGAP, but there was no significant difference between them. Mohammed et al. (18) reported that RTS, MGAP, and GAP had good discriminatory ability in predicting the mortality of adult multiple trauma patients. The AUROC was 0.879, 0.890, and 0.881 for MGAP, GAP, and RTS, respectively, whereas there were no statistical differences between the three scoring systems. These findings were consistent with those of the present study.
In this study, the survived and non-survived patients had significant differences in age, SBP, and GCS, which are the components of GAP and MGAP. RTS ignores the impaired physical resilience associated with aging, and this could be the possible reason for the superiority of GAP and MGAP over RTS in some previous studies (11,17). MGAP and GAP could be more accurately used for injured patients in moderately resourced trauma centers at the time of hospital arrival rather than at a delayed time (18).
Galvagno et al. (19) compared MGAP and RTS to predict in-hospital mortality in trauma patients. They suggested that the MGAP could be a preferable and more easily calculable pre-hospital scoring system. Jeong et al. (20) reported that the accuracy of GAP for the prediction of in-hospital mortality was similar to that of MGAP and significantly better than that of RTS.
Similar to the present study, Yadollahi et al. (3), Soltani et al. (10), and Rahmani et al. (9) showed that there is no significant difference between GAP and MGAP as predictors of mortality in multiple trauma patients. Indeed, the trauma mechanism did not affect the accuracy of scores or patient outcomes. Kondo et al. (13) found that GAP predicted mortality more accurately than MGAP in ED settings. No trauma mechanism score may be effective without an anatomical score. In addition, penetrating trauma subjects comprise less than 10% of the trauma population (3,13,16).
This study found that MGAP and GAP scores can be used as a powerful scoring system for evaluating patient survival in the ED setting. In addition, because of ease of use, the GAP score is more acceptable than MGAP in the triage of trauma patients.
In this study, GAP, MGAP, and RTS had high NPV and low PPV. This may be due to the low prevalence of 24-h mortality (7.2%). Prevalence directly affects NPV and NPV. A reduction in prevalence decreases PPV and an increase in NPV.
Study Limitations
This study has some limitations. First, the present study was retrospective. Second, it was conducted in a single center. Third, the sample size is small. Because the Poursina Hospital was a referral center for COVID-19 until March 2021 it was possible to collect samples from this date onward.
Conclusion
Rapid and accurate prediction of patients at risk of in-hospital mortality can improve patient outcomes. The RTS, GAP, and MGAP scores were good predictors of 24-h mortality, and they were similar in predicting early mortality in multiple trauma patients. The GAP score is easier to calculate and has fewer variables; therefore, it may be more beneficial to provide quick results and allow for quick decision making. It is a simple and rapid score that can be used for the timely triage of multiple trauma patients in the ED. An early calculation of the GAP score in the triage unit can help allocate needed resources earlier to patients at a higher risk of death and lead to improved trauma management.
Ethics
Ethics Committee Approval: The study protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1400.519, date: 26.01.2022).
Informed Consent: Retrospective cross-sectional study.
Peer-review: Externally and internally peer-reviewed.
Authorship Contributions
Concept: P.A., S.M.Z.Z., F.H., P.M., E.E., N.N.R., Design: P.A., S.M.Z.Z., F.H., P.M., E.E., N.N.R., Data Collection or Processing: P.A., S.M.Z.Z., F.H., P.M., E.E., N.N.R., Analysis or Interpretation: P.A., N.N.R., F.H., Literature Search: P.A., S.M.Z.Z., F.H., P.M., E.E., N.N.R., Writing: P.A., S.M.Z.Z., F.H., P.M., E.E., N.N.R.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.